Socialized Medicine in America: The Veteran’s Health Administration and TRICARE
God Bless America, and God Bless Our Troops
America, the land of the free BECAUSE of the brave. Defeating the Nazis and Imperial Japan in World War Two, fighting to contain Communism in the Korean peninsula and Vietnam, and defending the free world from the terrors of the Soviet Union and their tyrannical socialist economy. Because of their patriotic commitment to our cause, the United States Government has committed itself to caring for these soldiers via pensions, education, subsidized loans, and socialized medicine. That’s right, capitalist America has a true socialist health care system paid for, owned, and operated by the federal government; doctors and all. The Veteran’s Health Administration (VHA). That’s today’s topic.
Origins
The United States has tried to care for veterans since the very start of our nation. After the Revolutionary War, pensions were offered to disabled veterans, while medical care was mostly left to states and local communities. However by 1811, the federal government opened the first medical facilities for veterans. Benefits and pensions were also offered to widows and dependents over time, not just the veterans themselves. After the Civil War, many domiciliary homes were opened for veterans, and medical and hospital care was often offered even if their service was not the original cause for the condition.
In response to the US entry into World War One, Congress expanded programs for veteran disability compensation, insurance for personnel and veterans, and rehabilitation for the disabled. As a result of this action, veterans had three separate government agencies: the Veterans Bureau, the Bureau of Pensions of the Interior Department, and the National Home for Disabled Volunteer Soldiers. After The Great War ended, these agencies were consolidated into the Veteran’s Bureau in 1921. Public Health Service Veteran’s Hospitals were placed under the bureau’s management, and the government undertook further hospital construction to meet the demand from America’s new veterans. Care expanded throughout the 1920s to cover non-service-related health care needs, to take care of patients wounded by mustard gas, tuberculosis, and began to cover women as well. In 1930, President Hoover made the Veteran’s Bureau a proper federal agency and renamed it the Veteran’s Administration (VA). The VHA continued to grow, and by 1948 it had 125 hospitals under its umbrella.
In 1988, President Reagan elevated the VA to a cabinet-level department, and in 1991 the VA’s Department of Medicine and Surgery was redesigned and given the new name of the VHA. The VHA continued to grow, expand service to include treatment such as telehealth, and is an important aspect of training our medical specialists today. Approximately 60% of medical residents obtain at least some training at a VA hospital.
Overview
The VHA is the largest integrated health care system in the United States, serving 9 million veterans across the country with 171 VA Medical Centers, 1,113 outpatient centers, 371,000 health care professionals, and 113,000 medical trainees. They can serve veterans for a variety of services: surgeries, critical care, mental health care, orthopedics, radiology, physical therapy, cover pharmaceuticals, etc. It can also be stacked with other coverage like private insurance or TRICARE. In Fiscal Year 2022, VHA resources were listed at $128 billion. And with the passage of the PACT Act of 2022, this cost is only slated to grow.
VHA cost-sharing is set up via priority groups and number of visits. Visits to urgent care clinics can be free up to $30.
Outpatient rates can be a bit more expensive.
VHA inpatient copays can be quite expensive if your disability rating isn’t high enough, otherwise it could be free.
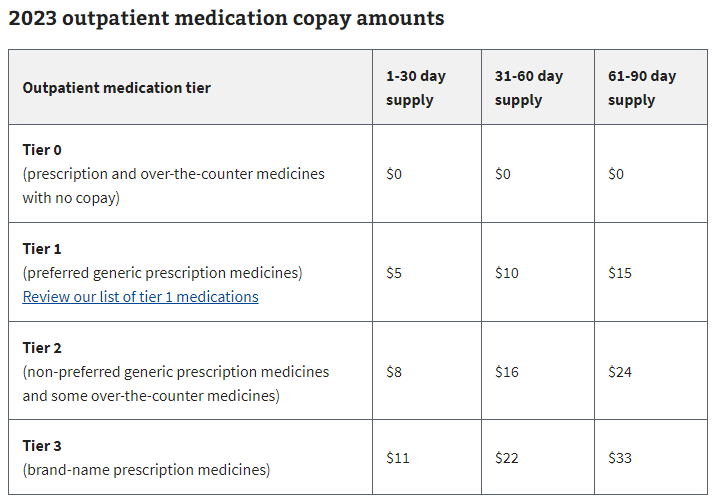
Like private insurance, VHA care uses drug tiers to set copay rates. Though VHA drug copays can be quite generous relative to private rates.
TRICARE
But the VHA isn’t the only way we care for veterans and service members. We also allow them to purchase private subsidized plans to get the care they need outside the VA and military health systems, called TRICARE. TRICARE can cover active-duty service members and their families, the National Guard, Reserves and family, retirees and family, survivors, and some former spouses. It can cover medical insurance, prescriptions, dental, and vision coverage. TRICARE has open enrollment periods just like Obamacare and Medicare, and there are a variety of plans and plan types to choose from.
Premiums rates for TRICARE can be quite low, with monthly rates cheaper than many people would find on Obamacare, Medicare, or many employer plans.
Cost-sharing on TRICARE also tends to be lower than what you would find with other types of commercial insurance or Medicare. The typical deductible or out-of-pocket maximum can easily reach into the thousands of dollars, but TRICARE offers far lower costs for enrollees.
Quality and Wait times
A common critique of the VHA is that while it is cheap and fully integrated, veterans that use it have to deal with low quality care, denials of coverage, and much longer wait times than they would on the commercial market. But is this true?
According to a RAND study comparing the VHA to commercial HMOs, Medicaid HMOs, and Medicare HMOs across 16 measures of quality of care in the outpatient setting, 6 in the inpatient safety measures, 3 mortality measures, and 17 inpatient effectiveness measures. The VHA outperformed Medicaid HMOs and commercial HMOs in all 16 outpatient quality measures! The VHA outperformed Medicare HMOs in 14 of 16 outpatient quality measures. For the inpatient setting, the VHA outperformed the competition in all 6 inpatient safety measures, all mortality measures, and 12 of the inpatient effectiveness measures. They performed worse on 3 readmissions measures and 2 effectiveness measures. The VHA also had lower variation in quality of care compared to these providers, indicating more consistency. A systemic review of studies found similar findings that the VHA often outperformed other models, though not always.
This could all be for naught if patients have excessive wait times for care. However, VHA wait times have been much shorter than commercial insurance in recent years. VHA hospitals had a mean wait time of 17.7 days to commercial wait times of 29.8 days in 2017. The only specialty with longer wait times through the VHA was orthopedics. However, wait times in the South are a bit longer than in other regions. Though wait times in the VHA were longer as recently as 2014, it appears they have made improvements in recent years while the commercial sector has stagnated. Just like the private sector, the VHA may go through periods of underinvestment and renewal.
Conclusion
So, despite arguments against socialized medicine and decrying socialism at home and abroad, our own soldiers and their families receive care from just a system, covering 9 million Americans for decades in one of the world’s largest integrated health care systems. Its cheap, appears to be relatively high quality, and wait times are now shorter than in the private sector. It even outperforms other types of public insurance like Medicare and Medicaid. Perhaps the challenge with systems like the VHA or Britain’s National Health Service stem not from the flaws in a socialized medical system, but in whether a country is willing to invest what it must to ensure that system is well run?










As a veteran, thanks for this thorough writeup. Highlighting something anyone in healthcare long enough should grasp - our public+private experiment is a hotmess. Health is a public issue and a human need.
🙌🏻
👏👏👏